AdventHealth on Tuesday broke ground on a new state-of-the-art building that will serve as Florida headquarters for Rothman Orthopaedic Institute.
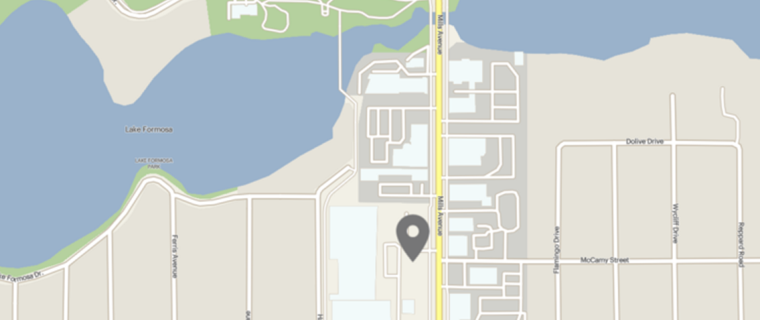
At 12 stories and 300,000 square feet, the building will be a major addition to the Orlando skyline, located next to Interstate 4 just north of the Princeton Street exit in the Health Village.
“Our community is growing, and we are seeing an increasing need for specialized care,” said Dr. Duane Davis, chief physician executive of the institutes for AdventHealth’s Central Florida Division. “This building will allow us to expand our services, bringing world-class clinicians together in a single, convenient location.”
In addition, the tower will include space for other AdventHealth services including neuroscience, imaging, rehabilitation, and research, offering comprehensive outpatient care, all in one convenient location.
“This project will have a big economic impact, both in construction jobs and in bringing more high-paying medical jobs to downtown Orlando,” said Orlando Mayor Buddy Dyer.
The tower is slated to open in late 2022.
Source: Fox35 Orlando