More than 800 hospital employees and 250 physicians will work at the new 424,000-square-foot facility. The facility includes an 85,000-square-foot medical arts building.
A recent $16M donation will be used to build an expanded breast health center as part of Sarasota Memorial’s Jellison Cancer Institute.
In 2021, Alabama construction firm Robins & Morton opened an office in Tampa, its third in Florida, to serve the growing demand for hospital construction here. The firm had seen requests for proposals triple from 2019 to 2020. The company’s health care revenue from Florida grew 30% in a four-year span.
Credit the gains to a substantial trimming of Florida’s certificate of need requirement in 2019. The action has produced a surge in health care construction around Florida.
“Since (the) Florida Legislature repealed part of the certificate of need law several years ago, we have seen increased demand for health care construction across the state, especially in acute care and specialty care facilities,” says Derek Gregg, a Robins & Morton vice president based in the firm’s Orlando office.
The certificate of need process required hospitals, home health care agencies and other providers to demonstrate that a new facility or service was needed and wouldn’t take business from existing players.
In Florida and other states, the law dated to the 1970s once the federal government made a certificate of need program a condition of receiving federal funding. The idea was to contain health care costs by preventing unneeded equipment and facilities. Guaranteeing existing players a market — they could object to a competitor’s application to expand — also was intended to subsidize indigent care.
Congress repealed the mandate in 1986, but certificate of need — much loved by entrenched providers — lived on in Florida and other states. That changed over time. A U.S. Federal Trade Commission study found certificates of need generally didn’t contain costs. Benefits provided were outweighed by the anti-competitive costs.
Florida got rid of certificates of need for home health agencies in 2000. In 10 years, the number of agencies doubled. Repeal of the requirement on other health care services followed. Then in 2019, the Legislature abandoned certificate of need for hospitals.
In the four years up to that point, the dollar value of hospital construction in Florida was $5 billion, according to data from Richard Branch, chief economist for the Bedford, Mass.-based Dodge Construction Network. In the four years following the repeal, the total reached $6.5 billion.
Health care systems expanded to gain market share in their regions and new regions of the state while out-of-state players planted flags here. A larger geographic footprint gives systems more leverage in negotiations with insurers. Where they located came down to “where the money is,” says Steven Ullmann, a professor in the Department of Health Management and Policy at the Miami Herbert Business School at the University of Miami. Thus, Palm Beach County has seen entrants from Broward, Miami-Dade, the northeast U.S. and Tampa while the surge bypassed rural and low-income markets.
From 2020 to 2022, healthcare companies announced at least 65 new hospitals in Florida, KFF HealthNews reported last year, up from 20 new ones from 2016 to 2018.
The dollar value of Florida hospital construction peaked in 2020 at $1.8 billion, more than double the annual figure from 2016, according to Dodge. Since then, new construction has remained above pre-repeal levels but has ebbed and flowed. Robins & Morton reports that the number of requests for proposals it’s receiving has stabilized.
The University of Miami’s Ullmann says that’s to be expected. “There’s only so much market out there.”
Even so, hot pockets of hospital development remain. In Plant City in eastern Hillsborough County, BayCare Health Care is replacing a 71-year-old hospital that has run out of room to expand any further. Since opening in 1953, the old South Florida Baptist Hospital has been expanded or renovated a dozen times, but it has maxed out its property and the Plant City area’s population keeps growing. So BayCare is building an entirely new South Florida Baptist Hospital that’s 68% bigger four miles away.
BayCare, which operates 16 hospitals in Pinellas, Hillsborough, Pasco and Polk counties, also is planning a 17th hospital in northern Manatee County. BayCare Hospital Manatee is slated to open in 2027. The building itself is currently in the design phase, so square footage and number of patient rooms are not finalized. The building permit application requests up to 207 private patient rooms, but the initial construction likely will have a smaller bed count.
HCA Florida Healthcare also has plans to construct a hospital in northern Manatee. The 150-bed hospital will serve as an anchor for the North River Ranch Village Center, a “healthoriented” complex that developer Neal Land & Neighborhoods is planning on 2,000-plus acres in fast-growing Parrish. No set timeline has been announced for the project.
WESLEY CHAPEL HOSPITAL
Wesley Chapel
BayCare Health System opened its $246-million Wesley Chapel hospital in 2023. It’s one of a slew of facilities that have sprung up across the state since the Legislature deregulated new hospital construction.
ALAN B. MILLER MEDICAL CENTER
Palm Beach Gardens
Universal Health Services broke ground last year on a 150- bed hospital in Palm Beach Gardens. The Alan B. Miller Medical Center, named for the founder and executive chairman of UHS, is sla1ted to open in 2025. UHS also owns the Wellington Regional Medical Center.
ORLANDO HEALTH WIREGRASS RANCH HOSPITAL
Wesley Chapel
Orlando Health is expanding its hospital footprint across I-4, with facilities slated for fast-growing portions of Pasco and Polk counties. Construction is underway in southeast Lakeland on Orlando Health’s 302-bed Lakeland Highlands Hospital, with an opening anticipated in 2026. Orlando Health is continuing site work for its 300-bed Wiregrass Ranch Hospital in Wesley Chapel. An opening date has not been announced.
SOUTH FLORIDA BAPTIST HOSPITAL
Plant City
The original South Florida Baptist Hospital had 250,000 square feet and few private rooms. Its $326-million replacement will have 420,000 square feet, six floors and 146 private rooms.
For Some, Permission Slips Still Apply
While Florida jettisoned its certificate of need process for hospitals in 2019, nursing homes, freestanding hospice facilities and other types of long-term care facilities still require the state’s stamp of approval. Florida is one of only 13 states, in fact, that regulates hospice services via a certificate of need process, according to a 2023 Florida TaxWatch report.
Source: Florida Trend
In Weston, a developer is requesting permission to build a six-story assisted living complex.
On April 15, the City Commission will take a look at the site plan and rezoning request for the 6.17-acre property located at 357 Racquet Club Road. The property’s rezoning application was initially presented to the City Commission in January, but it lacked a site plan that detailed the detailed development strategy. This is the first vote on the site plan and the second reading for the rezoning.
SREH-357 Racquet Club LLC, managed by Terry Salzman of Salzman Real Estate Advisors in Dania Beach, claimed in their most recent site plan application that the facility would have 245 senior housing units totaling 303 beds and 325,808 square feet. There would be 113 independent living units, 108 assisted living units, and 24 memory care units. A wide range of senior living amenities would be included, including a game room, eating area, theater, garden, exercise center, library, and swimming pool. The project would contain 200 parking places, based on the site plan. The sizes of the rooms would be 546 to 1,330 square feet.
The developer is requesting that the property be rezoned from “commercial” to “mid-rise multifamily.” Currently, it houses a 9,000-square-foot facility that was formerly the management office and welcome center for the nearby Vacation Village timeshare complex, which was built in 1975.
Fort Lauderdale-based Synalovski Romanik Saye designed the project.
Source: SFBJ
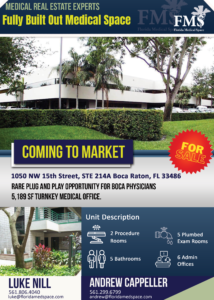
A highly focused and specialized team of marketing, leasing, and investment professionals at your service to represent your medical real estate needs so you can focus on what matters most. At Florida Medical Space, we understand that medical professionals have enough on their plates without worrying about office logistics. That’s why we’re thrilled to introduce our ready-to-move-in office spaces, designed specifically with the needs of healthcare providers in mind. But what makes our premium office spaces stand out from the rest? Let’s dive in and find out.
Why Choose Ready-to-Move-In Offices?
Imagine walking into an office that’s fully equipped, beautifully designed, and ready for you to start seeing patients on day one. That’s the convenience we offer. Our ready-to-move-in offices aren’t just about saving you time and hassle; they’re about providing a space that reflects the professionalism and care you bring to your practice. From advanced medical facilities to inviting and comfortable patient waiting areas, every aspect of our offices is curated to enhance patient care and streamline your operations.
Location and Accessibility
Located in the heart of accessible areas, Florida Medical Space ensures your office is not just a place to work but a convenient and easy-to-find destination for your patients. Proximity to rooftops, hospitals, pharmacies, and public transport links are just a few of the factors we consider to boost your practice’s visibility and accessibility.
State-of-the-Art Facilities
Our locations are handpicked to support a wide range of medical specialties. Whether you require advanced imaging equipment or specialized treatment and procedure rooms, we have spaces designed to cater to the unique needs of your practice.
Flexible Design and Layouts
Understanding that no two medical practices are the same, we offer various medical space options to suit your specific needs. Whether you need multiple consultation rooms, large treatment areas, or private offices, our team works with you to create a layout that maximizes efficiency and patient comfort.
The Florida Medical Space Difference
What truly sets us apart is our commitment to providing personalized solutions for every client. At Florida Medical Space, we’re not just offering office space; we’re offering a partnership. We take the time to understand your practice’s unique needs and preferences, ensuring your office is not just a space but a reflection of your dedication to patient care.
Tailored Office Solutions
From the initial consultation to the day you move in, our team is dedicated to crafting an office solution that aligns perfectly with your vision. We consider every detail, from the layout of your space to the specific amenities you need, to create an environment that enhances your practice’s efficiency and patient experience.
Unparalleled Support Services
Beyond the physical space, at Florida Medical Space we pride ourselves on the comprehensive support services available to all tenants. Recognizing that medical professionals should focus on their patients rather than administrative or logistical issues, we offer a range of services including:
Development Services:
Turn-key solutions from concept to operation. Specializing in healthcare real estate, our team collaborates with hospitals and medical groups to overcome financial and logistical challenges, ensuring your project is delivered cost-effectively and on schedule.
Tenant & Buyer Representation
Specializing in healthcare real estate, we ensure your practice finds its perfect Florida location. Benefit from our aggressive negotiations and zero-cost services, saving time and money. Our expert team uses in-depth market analysis to secure the best terms for your lease or purchase.
Leasing and Sales
FMS stands out by acting as a strategic intermediary, ensuring mutual objectives are met for both parties, leading to successful transactions. Our comprehensive approach includes market studies, targeted outreach to local physicians, and extensive marketing efforts, all aimed at achieving above-average leasing success and occupancy levels.
Niche Services
Catering to the unique demands of the senior living, addiction treatment, veterinary, and dental sectors, FMS stands as the premier source for tailored real estate strategies. Our dedicated divisions understand the intricacies of each specialty, from zoning for addiction treatment facilities to the specific space needs of veterinary offices. FMS empowers clients with knowledge on market dynamics, helping you make informed decisions on buying vs. leasing and navigating the competitive landscape.
Success Stories
Don’t just take our word for it. The success stories of our clients speak volumes about the benefits of partnering with Florida Medical Space. From pediatric clinics to specialized surgical centers, our clients have seen significant improvements in their operations, patient satisfaction, and overall success. These testimonials highlight the positive impact of moving to our premium office spaces, underscoring our commitment to supporting medical practices in their growth and development.
Conclusion
Choosing Florida Medical Space means opting for convenience, quality, and support. Our premium, ready-to-move-in medical real estate properties are designed with the needs of medical professionals in mind, providing a seamless transition and a solid foundation for your practice to thrive. With state-of-the-art facilities, tailored solutions, and a supportive community, we’re more than just a space provider – we’re your partner in success. Experience the difference that a premium medical office space can make for your practice and join the Florida Medical Space family today.
FAQs
1. What types of medical practices can benefit from Florida Medical Space’s offices?
Our offices are designed to accommodate a wide range of medical specialties, from family medicine to specialized surgical practices. Our flexible design options ensure that we can create a space that meets your specific needs.
2. How long does the setup process take?
The timeline can vary depending on the level of customization required. However, our team works efficiently to ensure your space is ready as quickly as possible, typically as soon as one month if we can identify a turn-key office solution for you. Custom offices can be built in as little as six months.
3. Are there any additional costs involved in customizing my office space?
We provide a detailed analysis of your total real estate costs before any property is chosen. We try to maximize transparency so you can make informed decisions about your space.
4. Can I expand my office space as my practice grows?
Florida Medical Space professionals will help understand your growth plans over the next three to five years and attempt to negotiate lease terms that allow flexibility. When purchasing real estate, it is important to buy property that accounts for future growth plans.
5. How do I get started with Florida Medical Space?
Simply contact us to schedule your initial consultation. Our team is ready to guide you through the process, from selecting your space to moving in. There is no up-front cost to leverage our years of medical real estate experience to identify a turnkey, move-in ready office that will meet your short and long-term needs.
Email: [email protected]
Office: (954) 346-8200